
Welcome to our public policy resource page! Long-term supports and services (LTSS) is a complex and growing sector of our health care system. When it comes to policy decisions, we know it’s important to understand the social and governmental issues surrounding LTSS in Kansas. Below is a list of helpful resources you can explore, and if you have questions about our field, we are happy to assist! Contact Rachel Monger, Vice President of Government Affairs, at [email protected]
Aging Demographics in Kansas
By the end of the next decade, 1 in 4 people will be over the age of 65 in two-thirds of Kansas counties. The rapid demographic shift in our state and will require new thinking around our state’s economy, infrastructure and budget. It will also bring to the forefront many issues that touch Kansans’ everyday lives, such as housing, transportation, social and civic engagement, family caregiving, community support services, health care, and dementia-friendly communities.
The Center for Economic Development and Business Research (CEDBR) at Wichita State University provides many helpful demographic tools. Wondering how many people are (or will be) over the age of 65 in your county? Check out this page on the CDEBR website.
Check out the 2025 “aging map” of Kansas created by WSU for a sobering look at how fast our older population is growing in Kansas.
The Landscape of Aging Services in Kansas
Researchers at the AARP Public Policy Institute release various reports on heath and housing for older people, as well as LTSS services available in every state. Some recent publications that you may find helpful:
Did you know that LTSS providers are the second largest health care employer in our state? Our field employs more than 55,000 people across Kansas, and indirectly contributes an additional 23,000 jobs to the Kansas economy. Source: Kansas Hospital Association: The Importance of the Health Care Sector to the Kansas Economy January 2020 Report
For more details about LeadingAge Kansas members, and their role in Kansas LTSS, check out our Aging Quick Facts brochure.
The Cost of Long-Term Care in Kansas
The following is the average annual cost of LTSS in Kansas:
- Home Health: $52,624
- Adult Day Services: $19,500
- Assisted Living: $48,612
- Nursing home care with a semi-private room: $90,155
- Nursing home care with a private room: $102,200
Source: Genworth Cost of Care Survey 2019
The Elder Index is a free online resource available for anyone to look up customized information about the cost of elder living in any county, state or the country.
Medicaid and Medicare
Many people are unaware that Medicare DOES NOT pay for long term supports and services. It may cover short term services after a major medical event, but assistance with long term medical conditions or activities of daily living are not covered.
Medicaid pays for more than 50% of nursing home care in Kansas. Why?
Without the assistance of Medicare, older people must pay for LTSS out of their own pockets. Once an older person spends down all their money and assets paying for LTSS, the older person is eligible for Medicaid coverage. At an average cost of $100,000 a year, most nursing home residents spend down their assets very quickly. This is why Medicaid pays for so much of nursing home care in our state.
Medicaid pays for two types of LTSS for persons over age 65: Nursing home care and home and community based services (HCBS). LeadingAge Kansas members provide both types of services.
In 2019, Medicaid covered 10,304 nursing home residents, and in-home services for 4,775 frail elders.
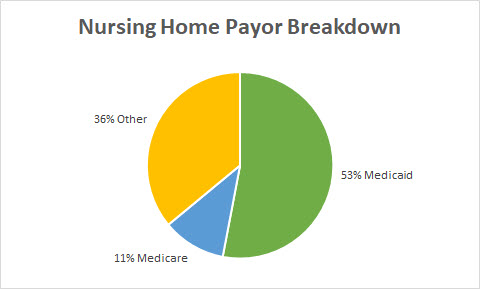
Nursing Home Payor Breakdown:
- 53% Medicaid
- 11% Medicare (Short-Term Rehab Stays)
- 36% Other (private funds, VA benefits, long-term care insurance, etc)
Medicaid does not pay for Assisted Living facilities, or any other “housing with services” models of long-term care. An older person in the Medicaid program may receive HCBS services while a resident in an assisted living, but Medicaid does not cover room and board or any other expense outside of approved health care assistance. For this reason, very few Medicaid recipients are in assisted living or other similar settings.
For more information on the Medicaid program in Kansas, check out the 2019 Medicaid Primer from the Kansas Health Institute
Adult Care Homes
Adult care homes are the most heavily regulated, and thoroughly inspected health care providers in Kansas, and the nation. In our state, adult care homes include nursing homes, long-term care units of critical access hospitals, assisted living facilities, home plus, residential health care facilities, and adult day care providers.
Laws and Regulations
All adult care homes are licensed by the state of Kansas, and are subject to Kansas adult care home laws and regulations. Adult care homes are regulated by the Kansas Department for Aging and Disability Services (KDADS), and all applicable regulations may be found on their website.
Nursing homes that care for people in the Medicare and Medicaid programs are also subject to federal laws and regulations governing long term care. They are regulated by the Centers for Medicare and Medicaid Services (CMS) housed within the U.S. Department of Health and Human Services. CMS recently overhauled nursing home regulations, adding even more requirements. The regulations may be found on the Code of Federal Regulations website.
Surveys and Enforcement Actions
All adult care homes are subject to annual inspections, also known as a “survey.” A home will receive additional surveys during the year if there are any reports made to KDADS that warrant an investigation at the home. All surveys are unannounced, and usually last 5-7 days. Surveyors conduct an in-depth look at the physical plant, observe resident care, inspect resident records, comb through administrative records, and conduct interviews with residents and staff.
Surveys are meant to uncover any non-compliance with state and federal regulations. Instances of non-compliance are written up in the survey results report as “deficiencies.” Each deficiency identified in the survey is also assigned a severity level. Severity levels range from “no harm” (the lowest) to “immediate and widespread jeopardy” (the highest).
All deficiencies must be resolved by the adult care home within a certain amount of time through a “plan of correction.” If the home receives a high severity level deficiency, it is also subject to fines between $100 - $10,000 per day, denial of payment for Medicaid and Medicare services, and/or a ban on new admissions to the home. An adult care home with poor surveys and continued non-compliance may have its license revoked by the state, and be forced to shut down.
Further Resources:
|